Enhancing the effect of cash buyback on the return of unused opioid pills

Target a priority outcome
Unused prescription opioid pills stored in the home can contribute to opioid abuse. It is estimated that between one quarter and three quarters of patients prescribed opioids either misplace unused pills or store them for future use, presenting a risk to those who may later find them.¹ Clinical practice guidelines issued by the Department of Veterans Affairs and the Department of Defense stress the importance of encouraging patients to return their unused opioid pills for proper disposal.² The White River Junction Veterans Affairs Medical Center implemented a cash buyback program, called “Cash for Your Stash,” in which patients who return unused opioid pills to the VA pharmacy can receive $5 per returned pill, up to $50.³ The program is offered to patients who receive one-time, short-term prescriptions for opioids to manage pain following outpatient surgery.
Translate behavioral insights
There are a number of potential barriers to returning unused opioid pills for patients. For one, it may simply be difficult for patients to remember that the Cash for Your Stash program exists, as they receive information about the cash buyback option in the recovery room following outpatient surgery, when they are under the influence of anesthesia. A week or more often goes by before patients know whether they have unused pills and can take action to return them. Inertia or lack of motivation may prevent patients from making the effort to return the unused pills, even if they remember that the option is available to them.
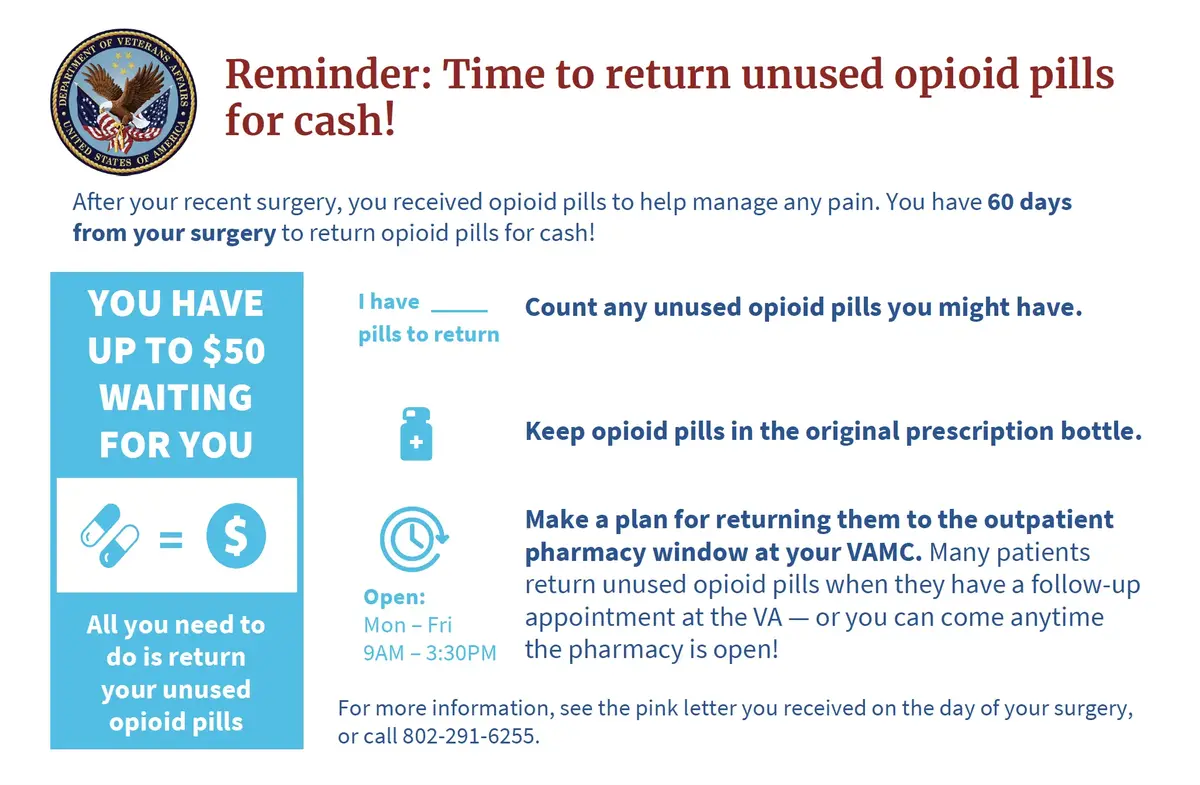
To address these barriers and enhance the effect of the cash incentive, we designed a treatment involving two reminder cards. One card is given to the patient when they receive their prescription opioid pills, and another is mailed to the patient approximately one week later. The cards were designed to make information available to the patient at a time when they can take action, and to motivate action by framing the incentive as money waiting to be claimed.⁴
Figure 1. Card mailed to treatment patients a week after surgery
Embed evaluation
The treatment was tested via a randomized evaluation. The project was implemented from June 2019 through January 2022, during which time 512 patients were offered the cash buyback (258 treatment, 254 control).⁵ Patients in the control condition received the standard information only, which included a printed page about the cash buyback option and a sticker on the pill bottle, shared with patients at the time of surgery. Patients in the treatment condition received the reminder cards in addition to the standard information about the buyback program. Patients were randomly assigned to treatment and control conditions by the week of their surgery; within each two-week interval during the field period, one week was randomly assigned to treatment, and the other to control.⁶ The COVID-19 pandemic canceled surgeries conducted at the White River Junction VA during this period; the program resumed once surgeries were rescheduled.
Analyze using existing data
We used existing administrative data from the VA electronic health records to compare the rates at which patients in the treatment and control groups returned unused opioid pills.⁷ We were also able to compare numbers of pills returned and the length of time from surgery to pill return. The data included patient characteristics, including age and gender, as well as information about the surgical procedure and the type and quantity of opioid prescribed; these additional data elements enable a more accurate and precise estimate of the impact of the cards.
Results
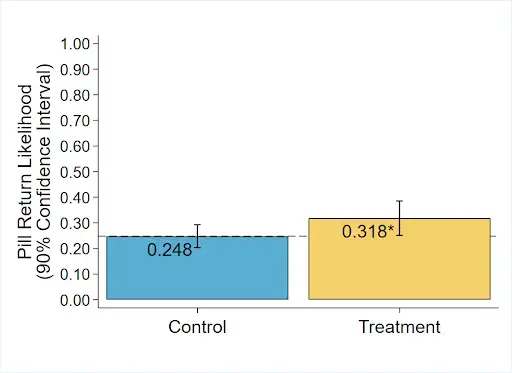
The treatment increased the likelihood that a patient would return unused opioid pills by 7.0 percentage points over a baseline of 24.8% in the control group (p = 0.043, 95% CI [-0.98, 15.01]).⁸ The treatment also increased the average number of unused opioid pills returned by 1.08 (p = 0.014, 95% CI [0.11, 2.04]) on a baseline of 2.08 pills, including patients who did not return any pills. The treatment did not have any statistically significant impact on the time from surgery to pill return.
Figure 2. Treatments increase the likelihood that patients return unused pills by 7.0 percentage points.
Build evidence
This evaluation demonstrated that reminder cards can significantly enhance the effectiveness of an overt financial incentive to return unused opioid pills for proper disposal. VA plans to continue using the cards as part of the Cash for Your Stash program in White River Junction, Vermont, and is exploring the possibility of adopting the cards in other locations where the program operates.
Additional cost effectiveness analysis indicated that the reminder cards reduced the cost per pill returned.⁹
- When using reminder cards, the cost per pill returned was $12.56.
- When no reminder cards were used, the cost per pill returned was $14.94.
Notes:
- U.S. Government Accountability Office (2019): Prescription Opioids: Patient Options for Safe and Effective Disposal of Unused Opioids (https://www.gao.gov/products/gao-19-650).
- US Department of Veterans Affairs and US Department of Defense (2017): Clinical Practice Guideline for Opioid Therapy for Chronic Pain. (https://www.healthquality.va.gov/Guidelines/Pain/Cot/Vadodotcpg022717.Pdf)
- Liu, Jean; et al. (2021). “Nudging patients and surgeons to change ambulatory surgery pain management: Results from an opioid buyback program,” Surgery. 170: 485-492.
- Kahneman, Daniel; Knetsch, Jack L.; Thaler, Richard H. (1990). “Experimental Tests of the Endowment Effect and the Coase Theorem”. Journal of Political Economy. 98 (6): 1325–1348.
- The stopping rule for the project was ultimately determined by factors related to project utilization. While the full results were not known, a midpoint analysis had already been conducted when the stopping decision was made.
- Thus randomization was by cluster within blocks, where clusters were weeks, and blocks were consecutive two-week periods.
- Unless noted otherwise, all of the analysis reported in this abstract was prespecified in an analysis plan, which can be found at oes.gsa.gov.
- Following the analysis plan, the standard errors were not adjusted for clustering. Doing so as a robustness check decreases the standard errors.
- These cost estimates include only running costs and specifically consider the costs, number of patients, and treatment effects observed at this clinic location.
